Continue reading "Fixing the NSW Workers Compensation Scheme"
Continue reading "Celebrating the Workplace Rehabilitation Industry"
Continue reading "New icare Claims Service Providers for NSW Workers Compensation Claims"
Continue reading "Work Options reappointed on icare Workplace Rehabilitation panel"
Continue reading "Why employee counselling (EAP) programs are not the total solution!"
Continue reading "The blueprint for managing mental health in your business"
Continue reading "Financial Incentives to help your Recruitment"
Continue reading "A Birthday cake and Mental Health, what could possible go wrong?"
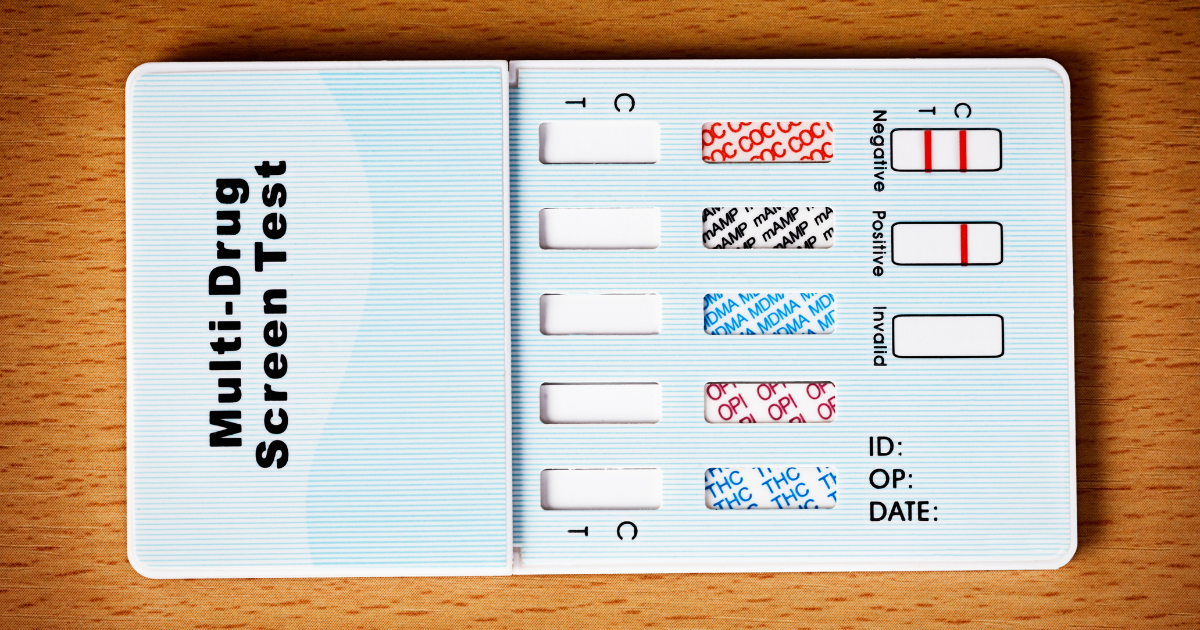
Continue reading "What is the top Drug & Alcohol testing question asked?"
Continue reading "Top 3 Mental Health resources to support your workers"
Continue reading "Our top tip for workers’ compensation claim success"
Continue reading "Why Drug testing is an investment and not a cost"
Continue reading "Steps in supporting your workers back to the workplace"
Continue reading "How to choose a Workplace Rehabilitation Provider"
Continue reading "Top 5 reasons for a pre-hire fitness assessment"
Continue reading "The Australian Health & Safety Business Podcast"
Continue reading "Experience of a work-from-home ergonomics assessment"
Continue reading "Qualities of the Mental Health Champion role"
Continue reading "Assessing fitness for work after an injury or illness"
Continue reading "Benefits of enlisting a Workplace Rehabilitation Provider"
Continue reading "What is a Workplace Rehabilitation Provider?"